Chronic Lymphocytic Leukemia Survivor
Finding a Silver Lining in a CLL Diagnosis
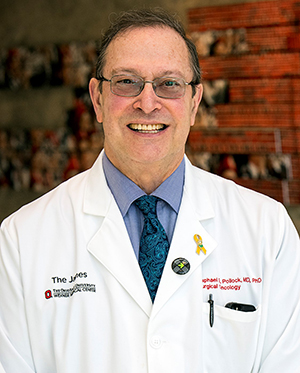 As a sarcoma surgeon and the director of The Ohio State University Comprehensive Cancer Center (OSUCCC), Dr. Raphael Pollock has always placed a high priority on building relationships with his patients. In 2017, he discovered a new and very personal way to connect — as a fellow cancer survivor.
As a sarcoma surgeon and the director of The Ohio State University Comprehensive Cancer Center (OSUCCC), Dr. Raphael Pollock has always placed a high priority on building relationships with his patients. In 2017, he discovered a new and very personal way to connect — as a fellow cancer survivor.
Right before the holidays in 2016, I took my son out to dinner, came home and fell asleep. I awoke about an hour later with intense abdominal pain. It was so bad I couldn’t fall back asleep. The next day was a fairly easy schedule, but by noon I felt so bad I had to go home. Again, I couldn’t sleep or keep anything down. After 48 hours, I went to the OSUCCC emergency center where they ruled out such things as a pulmonary embolism or a heart attack. My chest X-ray did have the appearance of pneumonia, and I was severely dehydrated, so I was admitted to the hospital. I stayed the weekend and was released with a follow-up scan scheduled for a few weeks later.
I got through the holidays just fine. However, by the second week in January, I had no energy and felt feverish. My follow-up scan was just four days away. On the day of the scan, I spent the day operating and then went for my appointment that evening. By the time I was done with my scan, rather than trying to find someone who could read the scan at that late hour, I logged in at home to read it myself. My first thought was
that someone had mis-labeled my scan test results because I was looking at an abdomen with a massively enlarged spleen. I did a self-exam and realized my spleen was enlarged, so I called a friend and colleague who is a hematologist-oncologist at OSUCCC. He reviewed the scan, and this is what he told me:
“Drive back to the hospital right now. Stay off the expressway. Use surface roads. And don’t use your seat belt. Your spleen is about to rupture, and you need an emergency operation to remove it.”
It did, in fact, rupture in the operating room, fortunately not until just after it was taken out. Even more surprising was that it contained a very large Listeria abscess infection that could have proved extremely serious had it ruptured in my body.
Funny enough, as I recuperated for the next five days in the hospital, I was on the same floor with four of my own surgical oncology patients on whom I had recently performed surgery. We took our walks around the floor together, IV poles in hand; it was a great bonding experience!
About two weeks into my recovery, a professor of hematology-oncology pathology who is a friend of mine called to discuss my pathology results and specifically mentioned that a chromosome 13q deletion had been found in my spleen. I asked why she was talking to me about a chromosomal abnormality that is frequently associated with chronic lymphocytic leukemia (CLL) and was answered with, “Didn’t they tell you? Your spleen was filled with leukemia!”
My friend and colleague who advised me to return immediately to the hospital the night of my scan is an international leader in research and treatment of CLL, and he became my physician. I had measurable disease on both sides of my diaphragm and, as a result, my CLL was considered fairly high-risk.
I was treated with a targeted therapy as a participant in a two-year clinical trial and did well on it. The amount of disease shrank, my white blood cell count decreased to near normal and the del 13q abnormality became nearly undetectable. The targeted therapy agent that I was receiving had a side effect of causing deep fissures in my fingertip skin. As a surgeon scrubbing my hands many times during the work week, this was a painful problem. I switched to a related but different targeted therapy, and the fissures promptly healed. Because of my residual disease, I anticipate staying on this therapy for the rest of my life. Other than cancer fatigue, I’m relatively asymptomatic. If I wasn’t occasionally fatigued, I might even forget I have CLL.
Although I’ve worked for decades with cancer patients and I come from a family of medical professionals, receiving my own diagnosis wasn’t easy. But I’ve found the silver lining. I’ve always understood the value of connecting with my patients. It’s one of my personal core values. But I’d never been able to relate from the perspective of a cancer survivor myself, only as a cancer care provider. Now when I talk with a patient about cancer fatigue, I can speak from personal experience because I have it myself. And I’ve always been a vigorous proponent of clinical trials because if nothing else, you are seen and examined by a large number of health care providers as well as helping to advance new possibilities in clinical care. So now when I recommend clinical trial participation, I can advocate from personal experience because I’ve been a participant.
My patients have told me that this new perspective of shared cancer experiences has deepened their trust in the authenticity of our doctor-patient relationship, and that is gratifying to me on so many levels.
As a doctor and a patient, I’ll offer this advice:
- Don’t let your cancer take any more of your life than it already has.
- Don’t be dominated by statistics. There is every reason to believe that you will become a long-term survivor.
- Any time you have a serious or potentially life-threatening illness, your chances are better that you’ll get cutting-edge treatment if you seek out a specialist. Something people don’t realize is that specialists aren’t just in major cancer centers. OSUCCC, for example, links to many smaller community hospitals. And with telemedicine, you have more accessibility to physicians who can help.


