Multiple Myeloma Survivor
Multiple Myeloma Survivor Beating the Odds
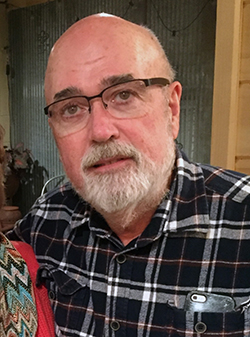 Paul Walker feels great, something he wasn’t so sure would be true after he was diagnosed with multiple myeloma in 2007. After two stem cell transplants and four relapses, he and his wife take life day by day and appreciate everything.
Paul Walker feels great, something he wasn’t so sure would be true after he was diagnosed with multiple myeloma in 2007. After two stem cell transplants and four relapses, he and his wife take life day by day and appreciate everything.
I thought I’d pulled a muscle in my left ribcage. It hurt more when I’d sneeze or cough, but I ignored it until I saw my family doctor a few months later. He thought it was a pulled muscle, too, but ordered a CT to be sure. His first diagnosis was lymphoma. Obviously, I didn’t like the sound of that. After another look, he changed the diagnosis to multiple myeloma, a disease I’d never heard of. He told me it was not curable, but treatable, with a typical prognosis of three to five years. That was scary.
I was referred to a hematologist and an oncologist. They ran more tests and found a tumor called a plasmacytoma on my right ribcage. The bone the tumor was sitting on was nearly eaten away by the myeloma. After I had radiation therapy to eliminate the tumor, the doctor told me he believed I had smoldering myeloma. He estimated I wouldn’t see any more signs of the disease for about five years. Imagine my surprise when just a few months later, my wife and I were in Hawaii and I felt pains up and down my spine. I saw my doctor when we got home and learned I had two compression fractures in my spine caused by the bone being weakened from the myeloma. On top of that, it had already become an overt Stage II myeloma.
I started on a bone-strengthening agent to help build up my bones. It helped a great deal with the pain from the compression fractures.
My doctor said it was on the “bad end” of Stage II, so I sought a second opinion at a prominent cancer center out of town. The doctors there agreed with the diagnosis and discussed my treatment options — stem cell transplantation or chemotherapy. Because I was only 55 and otherwise healthy, I chose to have an autologous stem cell transplant, which is a type of transplant that would use my own cells instead of a donor’s. The doctors explained the transplant process in great detail. They told me a stem cell transplant would be a temporary fix, and that some people need a second transplant after two years.
To reduce the cancer load before transplant, I was put on an oral drug that was a fairly new type of immunotherapy for myeloma, along with a steroid for four months. Then I went to the hospital for 16 days, where they harvested and froze my stem cells. Then, for two days, they gave me another drug to kill all my white blood cells, which made me vulnerable to infection. It made me very nauseated. My own cells were injected back in, and the nausea continued. I lost 20 pounds, but I never got a fever or infection. The doctor told me I should fight the urge to lie in bed after the transplant, so I started walking and using the exercise bikes on the hospital floor. I started slowly, sometimes just exercising five or 10 minutes a day. Three months later, I felt good, and I kept up the exercise, which I think really helps the healing process. I’ve taken an exercise class for cancer patients, and I volunteered in a clinical trial that focused on exercise for cancer survivors.
I had follow-up blood tests and bone marrow biopsies and, nearly two years later, I had a recurrence. I started on a clinical trial that was supposed to have a better version of the first drug I took in the hospital before the stem cell transplant, but it only worked for about 10 months before I found a tumor in my shoulder. We treated that with radiation therapy, and I started another drug. That worked well for about three years.
When my blood test counts began to rise, I had a second stem cell transplant. I relapsed three years later when a soft tissue tumor the size of an orange was discovered near my kidney. It was painful because it had wrapped around my sciatic nerve. Once again, I had radiation therapy to shrink the tumor, and that was successful. It was unusual for multiple myeloma to show up as a soft tissue tumor, and the doctor felt it put me at high risk for getting another tumor in six to 12 months. That was three years ago, and currently I feel great.
I don’t say I’m cured, but I do consider myself in deep remission. I’m on a low dose of the same immunotherapy I took before, and I still take a bone-strengthening agent every six months.
My wife has been my partner through it all. She took it on full charge, especially the stem cell transplants. She made sure everything in the house was clean, and she kept my exposure to germs to a minimum. She went with me to every appointment, asked questions and took notes. I wasn’t hungry, but I had to keep up my strength, so she experimented with recipes so I could force something down.
Support groups have been important to me. I met one woman who made a big impact on me. She had such a positive attitude. She shared her stem cell transplant experience with me and told me what to expect — the good and the bad — and that really helped to take the scare out of it.
I’ve had some setbacks, but I take it day by day. I see a lot of hope for the future in terms of new drugs coming out. I have five grandchildren and one on the way. I feel healthy, and I’m truly enjoying my life.


