Pain
Needle procedures to block pain
Procedures that are predominantly done through small entries into the skin, usually with a thin needle rather than through open surgery, are referred to as percutaneous techniques. These techniques are performed by an interventional radiologist, a pain physician or another interventionalist, doctors who specialize in these minimally invasive techniques that use imaging (X-rays, ultrasound and computed tomography [CT]).
Percutaneous techniques for pain management have provided pain relief for many patients with cancer-related pain. Often, pain relief is immediate. An important advantage is that these techniques are usually done in an outpatient setting, and patients can go home shortly after the procedure.
Percutaneous pain techniques include:
- Nerve blocks
- Ablative (removing of body tissue) procedures
- Vertebroplasty/kyphoplasty or cementoplasty (filling the bones of the spine with cement to stabilize them and/or reduce pain)
Nerve blocks
With a nerve block, a local anesthetic, usually with steroids, is injected around the nerve that travels to the painful area. The drugs stop the nerve from sending pain signals to the brain. The doctor will inject a small amount of a local anesthetic to numb the skin so there will be no pain where the needle is injected. Imaging helps the doctor insert the needle precisely. Before the nerve block procedure starts, a sedative may be given to help the patient become calm and relaxed, but oftentimes this is not required.
There are different types of nerve blocks, and they are named after the nerves that are treated. As described in more detail below, the common nerves that are blocked to treat cancer-related pain are the celiac plexus, the superior hypogastric plexus, and the lumbar and intercostal nerves, but many other nerves may be targeted, depending on the location of pain.
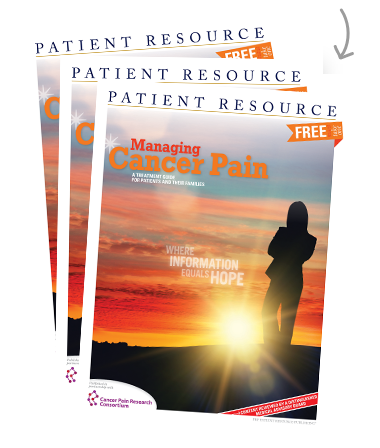
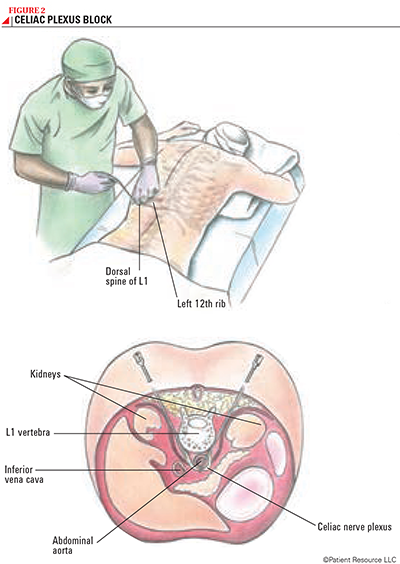
A celiac plexus neurolysis (interruption of the nerves) is usually done for people who have pain related to pancreatic cancer, as well as cancer of the bile duct, stomach or liver (see Figure 2). The superior hypogastric plexus is a web of nerves that travel to the pelvis. A nerve block in this location is usually done for pain related to advanced cervical, colorectal, prostate or testicular cancer. An intercostal nerve block is done to relieve pain in the upper chest or upper abdomen related to mastectomy or metastatic cancer to the ribs. Lumbar blocks (see Figure 1) or central epidurals are often done for patients with metastases to the spine with involvement of the nerves.
Many people with cancer-related pain have benefited from nerve blocks and have been able to reduce their oral pain medications. The length of time pain is relieved varies, but is usually a few months. Because the procedure is minimally invasive, the risks are relatively low, and the patient may be able to resume normal activities within a few days.
Ablative procedures
Ablative procedures kill painful tumor cells and can also be done with percutaneous techniques. With these procedures, heat, cold or a chemical solution is delivered through a thin needle to kill tumor cells causing bone pain, with the spine and the pelvis being the most common locations. Ablation with heat is radiofrequency ablation, or RFA; ablation with cold is cryoablation. Chemicals injected for ablation include highly concentrated alcohol or phenol.
As with other percutaneous techniques, the risk of side effects and complications is relatively low, and people can resume their usual activities within a few days. Ablative procedures have been effective in significantly reducing bone pain from metastatic disease and abdominal pain from cancer in the internal organs, with long-term pain relief reported. The procedure may be repeated, if necessary.
Vertebroplasty/kyphoplasty and cementoplasty
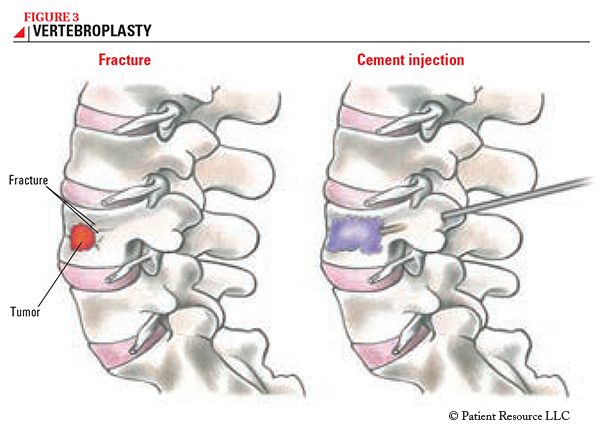
Percutaneous techniques are used in vertebroplasty/kyphoplasty, two procedures done to treat pain related to compression fractures of the spine caused by metastases. With vertebroplasty, bone cement is injected into the vertebral body (a bone segment of the spine) (see Figure 3). Sometimes, kyphoplasty is also done before vertebroplasty — this procedure involves placing a small balloon into the vertebral body and then inflating and deflating the balloon to create a cavity. This process can help to restore height to the vertebral body. When the bone cement hardens, it prevents further collapse of the vertebra, stabilizes the fracture, restores mobility and, in turn, relieves pain. As with other percutaneous techniques, the procedure is done with imaging guidance to ensure that the injection is precise. The risk of complications is low, and patients usually go home the same day.
Vertebroplasty, with or without kyphoplasty provides pain relief for most patients with cancer who have compression fracture of the spine. Often, back pain is relieved in just hours after the procedure. Cementoplasty involves putting cement in other bones fractured from cancer mostly in the pelvic bones for pain relief and fracture stabilization.
Deciding on an option
Many patients who have cancer-related pain can benefit from a percutaneous technique, but it is important to talk to your doctor about the benefits and risks of each procedure and if it’s the right procedure for your type of pain. If one of these procedures is not right for you, other options are available.