Small Cell Lung Cancer
Staging
Following diagnosis, your doctor uses a process called staging to better understand your type of cancer. Staging takes into account the size and location of the cancer and whether it has metastasized (spread) to nearby organs, tissues or lymph nodes, or to other parts of your body. Your doctor uses this information to develop a prognosis (outlook) and design a treatment plan, including identifying potential clinical trials that may be appropriate for you.
Staging provides a common language for doctors to communicate and collaborate on a patient’s cancer. For example, staging allows doctors to group patients who have a similar prognosis. This approach enables them to more accurately predict outcomes and help determine the type of treatment patients will receive.
To determine the stage of your cancer, your doctor will consider the results of the following:
- Physical exam.
- Laboratory tests of your blood, urine and body fluids.
- Imaging studies. A positron emission tomography (PET), computed tomography (CT) of the chest and magnetic resonance imaging (MRI) of the brain are routine.
- Tissue biopsy. Some biopsies are performed with a needle, although sometimes part or all of the tumor must be removed surgically to determine a diagnosis.
Doctors may use a combined staging approach to stage small cell lung cancer (SCLC), referring to the Veterans Administration Lung Study Group (VALSG) staging system as well as the American Joint Committee on Cancer's (AJCC) TNM classification and staging system.
VA Lung Study Group Staging System
The first staging system developed for SCLC is still the most widely used. The VALSG staging system divides SCLC into two stages: limited stage and extensive stage.
Limited-stage SCLC is confined to one part of the chest, in just one part of the lung and in nearby lymph nodes. Limited-stage cancers are considered to be Stages I to III of the American Joint Committee on Cancer (AJCC) TNM staging system.
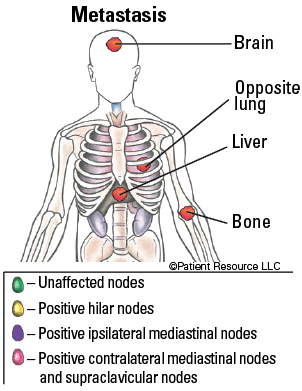
Extensive-stage SCLC has spread to other parts of the body, such as the area between the lungs or other lung, or outside of the chest, such as to the brain or bone. It is considered to be Stage IV in the AJCC TNM staging system.
AJCC TNM Staging System
Some doctors also consult the TNM (tumor, node, metastasis) system, developed by the AJCC and the International Association for the Study of Lung Cancer, to classify and stage lung cancer (see Table 1).
The T category identifies the primary tumor’s size and location. The N category indicates whether lymph nodes show evidence of cancer cells. If so, the location of these lymph nodes is important because it shows how far the disease has progressed. The M category describes distant metastasis (spread), if any. Cancer can spread by growing into nearby tissue, or traveling through lymph vessels or blood vessels to other parts of the body. An M subcategory may be added based on the presence of tumor cells that can be detected only by using a microscope.
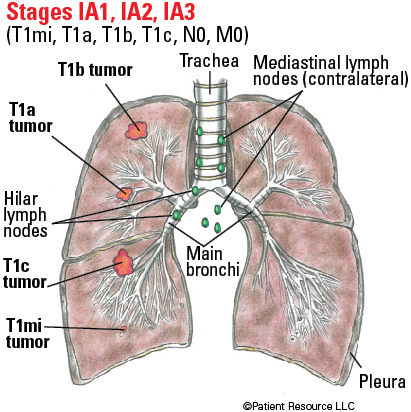
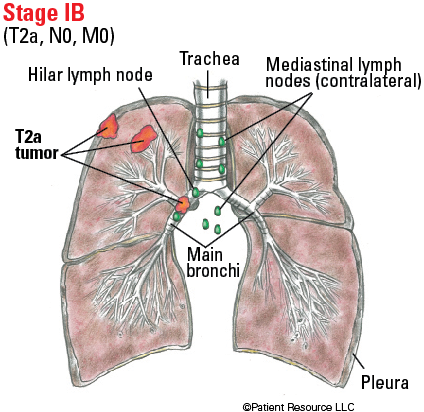
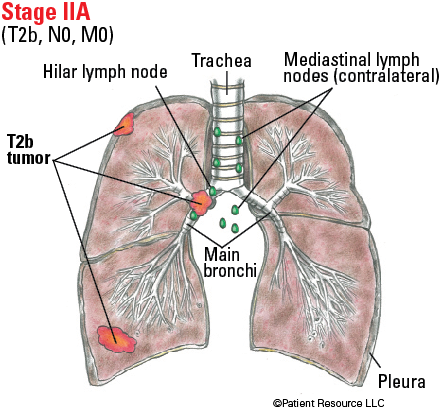
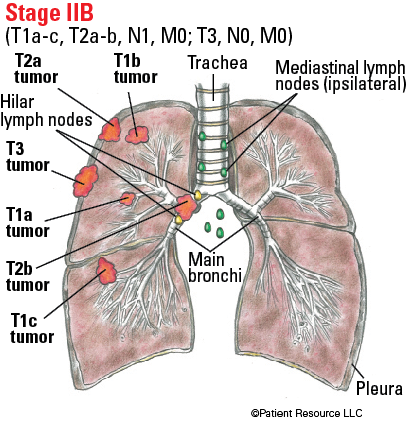
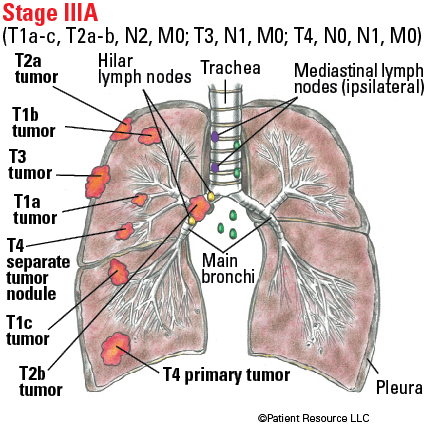
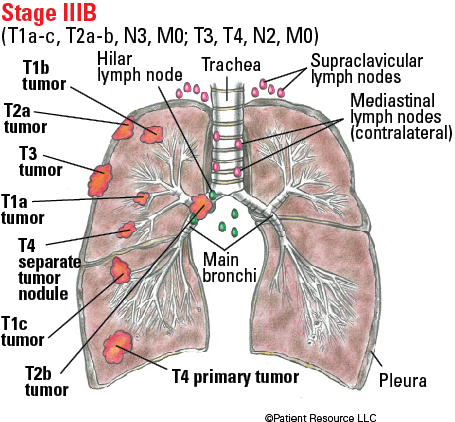
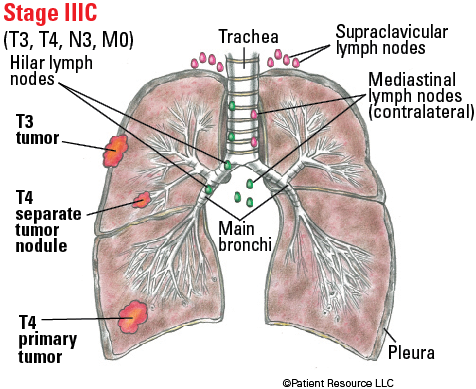
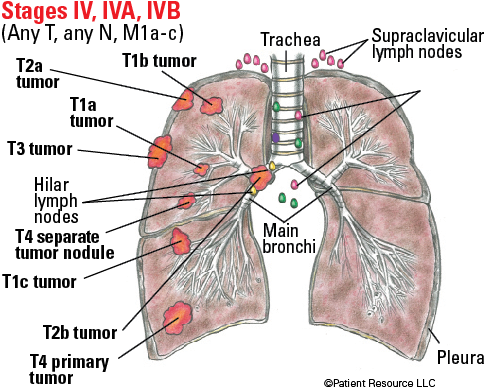
For illustration purposes, the tumors in Figure 1 are shown on one side of the lungs. They may, however, be present in any area of the lungs.
Staging combines the patient’s T, N and M status, then assigns a number (see Table 2).
- Stage 0, also known as in situ, is a precursor of an invasive cancer (not shown).
- Stages I and II are generally confined to the local area where the cancer is found, with or without adjacent lymph node involvement. They are treated as early stage and are considered potentially curable; therefore, every effort should be made to render a cure for these diagnoses.
- Stage III is considered locally advanced, still confined to the chest but having spread to regional lymph nodes outside the lung in the mediastinum.
- Stage IV is locally or regionally advanced disease that has spread to distant sites.
Table 1. AJCC TNM System for Classifying Lung Cancer
| Category | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed, or tumor proven by the presence of malignant (cancerous) cells in sputum (mucus that has been coughed up) or bronchial washings (cells collected from inside the airways) but not visualized by imaging or bronchoscopy. |
| T0 | No evidence of primary tumor. |
| Tis |
Carcinoma in situ.
Squamous cell carcinoma in situ (SCIS). Adenocarcinoma in situ (AIS): adenocarcinoma with pure lepidic pattern (on the alveolar lining), ≯ (not more than) 3cm in greatest dimension. |
| T1 | Tumor ≯ (not more than) 3 cm in greatest dimension, surrounded by lung or visceral pleura (membrane surrounding the lung), without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). |
| T1mi | Minimally invasive adenocarcinoma: adenocarcinoma (≯ [not more than] 3 cm in greatest dimension) with a predominantly lepidic pattern (on the alveolar lining) and ≯ (not more than) 5 mm invasion in greatest dimension. |
| T1a | Tumor ≯ (not more than) 1 cm in greatest dimension. |
| T1b | Tumor > (more than) 1 cm but ≯ (not more than) 2 cm in greatest dimension. |
| T1c | Tumor > (more than) 2 cm but ≯ (not more than) 3 cm in greatest dimension. |
| T2 |
Tumor > (more than) 3 cm but ≯ (not more than) 5 cm or having any of the following features:
• Involves the main bronchus regardless of distance to the carina (ridge at the base of the trachea), but without involvement of the carina. • Invades visceral pleura (membrane surrounding the lung). • Associated with atelectasis (collapse of part of the lung) or obstructive pneumonitis (inflammation of lung tissues) that extends to the hilar region, involving part or all of the lung. |
| T2a | Tumor > (more than) 3 cm but ≯ (not more than) 4 cm in greatest dimension. |
| T2b | Tumor > (more than) 4 cm but ≯ (not more than) 5 cm in greatest dimension. |
| T3 | Tumor > (more than) 5 cm but ≯ (not more than) 7 cm in greatest dimension or directly invading any of the following: parietal pleura (outer lung membrane), chest wall (including superior sulcus tumors), phrenic nerve (nerve that helps control breathing), parietal pericardium; or separate tumor nodule(s) in the same lobe as the primary. |
| T4 | Tumor > (more than) 7 cm or tumor of any size invading one or more of the following: diaphragm, mediastinum (area between the lungs), heart, great vessels, trachea (windpipe), recurrent laryngeal nerve (nerve that helps speech), esophagus, vertebral body, or carina (at base of the trachea); separate tumor nodule(s) in an ipsilateral lobe (lobe that is on the same side of the body) different from that of the primary. |
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N1 | Metastasis in ipsilateral (on the same side) peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. |
| N2 | Metastasis in ipsilateral (on the same side) mediastinal and/or subcarinal lymph node(s). |
| N3 | Metastasis in contralateral (on the opposite side) mediastinal, contralateral hilar, ipsilateral (on the same side) or contralateral scalene, or supraclavicular lymph node(s) (located above the collarbone). |
| Metastasis (M) | |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
| M1a | Separate tumor nodule(s) in a contralateral (on the opposite side) lobe; tumor with pleural or pericardial nodules or malignant pleural or pericardial effusion. |
| M1b | Single extrathoracic (outside of the lung) metastasis in a single organ (including involvement of a single nonregional node). |
| M1c | Multiple extrathoracic (outside of the lung) metastases in a single organ or in multiple organs. |
Table 2. Stages of Lung Cancer
| Stage | TNM classifications |
| Occult carcinoma | TX, N0, M0 |
| 0 | Tis, N0, M0 |
| IA1 |
T1mi, N0, M0
T1a, N0, M0 |
| IA2 | T1b, N0, M0 |
| IA3 | T1c, N0, M0 |
| IB | T2a, N0, M0 |
| IIA |
T2b, N0, M0
|
| IIB |
T1a or T1b or T1c, N1, M0
T2a or T2b, N1, M0
T3, N0, M0
|
| IIIA |
T1a or T1b or T1c, N2, M0
T2a or T2b, N2, M0
T3, N1, M0
T4, N0 or N1, M0
|
| IIIB |
T1a or T1b or T1c, N3, M0
T2a or T2b, N3, M0
T3, N2, M0
T4, N2, M0 |
| IIIC |
T3, N3, M0
T4, N3, M0 |
| IV |
Any T, Any N, M1
|
| IVA |
Any T, Any N, M1a or M1b
|
| IVB |
Any T, Any N, M1c
|
AJCC Illustrated Stages of Lung Cancer
KEY WORDS
Contralateral: on the opposite side as the primary tumor
Hilar lymph nodes: in the lungs, in the region where the bronchi, arteries, veins and nerves enter and exit the lungs
Ipsilateral: on the same side as the primary tumor
Mediastinal lymph nodes: between the lungs, in the part of the chest that lies between the sternum and the spinal column