Understanding the Genomics and Genetics of Cancer
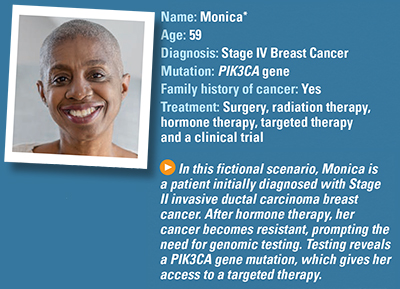
Fictional Case Study: Breast Cancer
What are Monica’s first symptoms?
One morning while showering, Monica feels an unusual lump in her right breast. She routinely does breast self-exams and has not felt this lump before. Her last mammogram did not detect any abnormalities. Concerned, she calls her doctor. He orders a new mammogram.
What is Monica’s diagnosis?
Results of the mammogram show a 22-millimeter lump. Her doctor also orders an ultrasound of the lump followed by a fine-needle aspiration biopsy. Biopsy results confirm it is breast cancer. Monica’s doctor refers her to a local oncologist.
The oncologist reviews the findings and orders a core needle biopsy with enough tissue to do additional testing for three main biomarkers: hormone receptor status (ER/PR) and HER2 status. The testing confirms that she has Stage II invasive ductal carcinoma breast cancer that is HR positive and HER2 negative.
The doctor asks her whether she has any history of cancer in her family. She does. Her older sister died of ovarian cancer at the age of 43 and her father died of lung cancer at 51. Because of this, he also orders germline genetic testing to see whether she has inherited a mutation that may be causing the breast cancer. Results show she does not have a mutated form of the BRCA1 or BRCA2 gene.
How will Monica’s breast cancer be treated?
Her oncologist recommends a partial mastectomy (also known as breast-conserving surgery) and a sentinel lymph node biopsy followed by radiation therapy and hormone therapy (an aromatase inhibitor). Her sentinel lymph node biopsy shows no spread to nearby lymph nodes.
What are the results of treatment?
Monica successfully completes treatment, continues on hormone therapy and is cancer-free for 2 years. At a follow-up appointment, she tells her oncologist she has had a persistent cough for several weeks. When her oncologist performs a physical exam, he notices a new lump under her right arm and asks her about it. She says it has felt a little tighter than usual but thought that was a long-term effect of radiation therapy. He orders new imaging tests, which show several lumps under her right arm and a spot on her right lung.
After performing biopsies of the lumps and the spot on her lung, he determines the cancer has returned. Her cancer is restaged to Stage IV.
What happens now?
Monica is alarmed that her cancer has spread. Her oncologist assures her there are options. He suspects the hormone therapy has failed and he wants to try to find out why. He wants to test her recent biopsy tissue for genomic mutations to determine whether she is eligible for more personalized treatments.
She asks her doctor to explain what genomic testing is and how it is different than the genetic testing she previously had. He explains that the initial testing was performed to find whether she had inherited a gene from her family that increased her risk of breast cancer. This testing looks specifically at the tumor tissue to find the mutations driving the growth of the cancer. He also says her recurrence and progression are likely caused by acquired mutations, which are not passed down from parents.
What are the results of her genomic testing?
Next-generation sequencing, which examines hundreds of genes, finds a mutation in Monica’s PIK3CA gene. The oncologist tells Monica that some patients who develop resistance to hormone therapy have a mutation in this gene. He reassures her that this means she qualifies for a type of targeted therapy known as a PIK3CA inhibitor that can be taken with an estrogen receptor antagonist.
How does she tolerate the new treatment?
Follow-up testing shows this treatment regimen is increasing her blood sugar levels. Her doctor explains this may indicate a need for more frequent blood tests. She also reports bouts of diarrhea that are difficult to control. He prescribes a medication to help. This intervention helps her tolerate the medication better, and her cancer stabilizes.
Sixteen months later, routine follow-up testing indicates her cancer returned. Her oncologist discovers her latest treatment is unable to control the cancer.
What are her options now?
The oncologist tells her that she may qualify for a clinical trial because other PIK3CA inhibitors are currently being tested. These new treatments may be able to control her cancer. Monica is eager to hear more and asks her doctor to help her find a clinical trial she may qualify for. He refers her to the cancer center’s clinical trials research coordinator, Janet.
Monica meets with Janet, who is able to find a clinical trial nearby that is testing another type of PIK3CA inhibitor. Monica is eligible for the trial, so after reading and agreeing to the Informed Consent form, she joins the trial.
She is responding well to treatment in the clinical trial. She is happy to be receiving the extra monitoring provided in the clinical trial and is excited that she is helping future metastatic breast cancer patients by participating in this study.
*Monica is not a real patient.