Understanding the Genomics and Genetics of Cancer
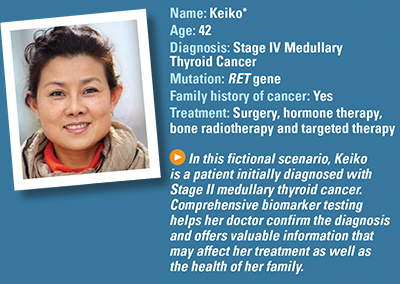
Fictional Case Study: Thyroid Cancer
How is Keiko diagnosed?
For four months, Keiko has noticed a swelling on the right side of her neck that moves when she swallows. Over time, it gradually enlarges but does not cause her any discomfort or pain and does not interfere with her swallowing. Still, concerned that it is not going away, she makes an appointment with her primary care doctor.
Her doctor is able to feel the lump and orders blood tests that show she has elevated levels of calcitonin and carcinoembryonic antigen (CEA), which may indicate cancer. She is referred to a head and neck surgeon.
The surgeon orders an ultrasound and a fine-needle aspiration biopsy of the lump. The ultrasound reveals a 2.5 centimeter tumor. Pathologic testing of the biopsy sample combined with the ultrasound imaging conclude she has Stage II medullary thyroid cancer. The doctor then orders comprehensive biomarker testing.
Keiko is unfamiliar with biomarker testing and asks her doctor to explain what it is and why he recommends it.
He explains that genomic testing is typically performed to identify mutations in blood or tissue samples. For thyroid cancer, it is used to determine whether she has medullary thyroid cancer, which can be inherited through a mutated RET gene.
What do the results show?
Keiko has a mutation in the RET gene. Because some medullary thyroid cancers are known to be inherited, he asks whether she has a family history of thyroid cancers. Keiko’s aunt had thyroid cancer, so genetic testing is ordered.
Results show she is also positive for the V804M RET germline (inherited) mutation, which can cause the growth of cancer cells. She also has multiple endocrine neoplasia type 2 (MEN2), a hereditary condition found in some medullary thyroid cancer patients who have a mutated RET gene.
This information allows him to counsel her about her family’s risk of other tumors, such as pheochromocytoma, and the risks of her family members developing cancer.
What is Keiko’s treatment plan?
Her doctor explains that although a targeted therapy to treat the RET mutation exists, it is only available if a patient cannot have surgery, or the disease is worsening or has spread to other parts of the body. As a result, she does not qualify for the targeted therapy at this time. The standard of care at Stage II is surgery to remove her thyroid.
Her surgeon recommends a thyroidectomy (complete removal of her thyroid) with a neck dissection to determine whether any lymph nodes are involved. Immunohistochemical staining is performed on the tumor, and it is positive for calcitonin, which is consistent with medullary thyroid cancer. None of the removed lymph nodes contain cancer cells.
After surgery, Keiko is prescribed thyroid replacement medication. She has routine monitoring blood work and imaging scans every three months.
Should her family members have genetic testing?
Yes. Because medullary thyroid cancer can be inherited, her doctor recommends that she encourage her family to get genetic testing. Her mother, father and sister are tested. Results show her sister also has the V804M RET mutation. She is referred to a thyroid oncologist for further evaluation and management.
What happens next?
Keiko will need follow-up testing for the rest of her life to monitor for recurrence. Ongoing monitoring will include testing her blood for biomarkers and checking her levels of calcitonin and CEA. Imaging scans will also be used.
What are the results of her follow-up testing?
Gradually, Keiko’s calcitonin and CEA levels begin to increase, indicating her cancer may be returning. During a physical exam, her oncologist feels a swollen lymph node on the right side of her neck. He suspects her cancer has returned and metastasized to a lymph node. She returns to her head and neck surgeon for a lymph node dissection. Testing of the lymph node shows it is positive for medullary thyroid cancer. Her disease has progressed to Stage IVA medullary thyroid cancer.
Despite removal of the cancerous lymph node, four months later, her calcitonin and CEA levels remain steady but have not decreased. Her doctor continues to monitor these levels.
About a year later, follow-up testing shows her calcitonin and CEA levels are increasing. An MRI shows multiple metastases in the cervical lymph nodes and bone lesions in the thoracic region of the spine.
How is her recurrence treated?
Keiko has external bone radiotherapy to reduce the bone lesions. Despite treatment, several months later, her calcitonin and CEA levels increase sharply. Her doctor reminds her of the targeted therapy for the RET mutation they discussed early on. He recommends treatment with a tyrosine kinase inhibitor.
She tolerates the targeted therapy well and continues having routine follow-up appointments to make sure her body is tolerating the drug. Her calcitonin and CEA levels decrease on this treatment, and her doctor is happy with the results.
*Keiko is not a real patient