Liver Cancer
Introduction
Receiving a liver cancer diagnosis is understandably troubling because, simply put, you cannot live without your liver. It is indispensable to your body, which makes it critical that you surround yourself with the best medical team and support system available. It may comfort you to know that new drugs, treatment strategies and clinical trials are making great strides in liver cancer treatment.
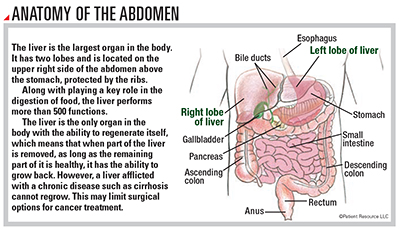
Primary liver cancer is a disease in which cancer cells form in the tissues of the liver. Cancer that develops in other parts of the body and metastasizes (spreads) to the liver is not primary liver cancer. It is considered the type of cancer from where it originated and is treated as such.
Liver cancer is a disease of the hepatobiliary (heh-PAH-toh-BIH-lee-ayr-ee) system. “Hepato” means liver, and “biliary” refers to the gallbladder and bile ducts. The two main types of primary liver cancer are hepatocellular carcinoma (HCC) and cholangiocarcinoma (also called bile duct cancer). Other types include angiosarcoma, a rare, aggressive form, and hepatoblastoma, the most common type of childhood liver cancer, usually affecting children 3 years or younger.
This content offers information about HCC, the most common type of liver cancer.
Understanding HCC
HCC begins in the hepatocellular cells of the liver tissue. You may hear it referred to as a disease within a disease because it is usually found in the presence of an underlying chronic liver condition. This makes it challenging to diagnose and treat. Less frequently, HCC can develop in an otherwise healthy liver.
The most common underlying condition of HCC is cirrhosis, which is scarring of the liver. Cirrhosis is a chronic, progressive disease that causes inflammation and irreversible damage as scar tissue slowly replaces healthy liver cells and the organ gradually loses function.
Another condition that is on the rise is nonalcoholic fatty liver disease (NAFLD), and its most severe form, non-alcoholic steatohepatitis (NASH), can also cause cirrhosis.
Viral hepatitis B and C, which are carried and spread through contact with blood and other bodily fluids, are also potential underlying conditions.
Higher incidence rates of HCC are found in people over the age of 60 and in Asians and Pacific Islanders, African Americans, Hispanics and American Indians/Alaska Natives. Although age and ethnicity are out of your control, you can make certain lifestyle changes related to diet, exercise, hepatitis B vaccinations and hepatitis C treatment that may reduce your chance of underlying conditions contributing to a liver cancer diagnosis.
The vast majority of patients do not feel symptoms related to HCC, but some that may rarely occur include the following:
- Bloating
- Decreased appetite
- Deep fatigue
- Feeling full despite eating less than normal
- Mild to moderate pain or tenderness in the upper right part of the abdomen or right shoulder
- Unintended weight loss
- Vomiting
When HCC becomes advanced and spreads beyond the liver (most commonly to the lung, abdominal lymph nodes or bone), multiple tumors may develop simultaneously and these symptoms may occur:
- Ascites (uh-SY-teez), swelling in the abdomen or legs
- Dark urine
- Light-colored stools
- Jaundice, causing yellow skin and yellowing in the whites of the eyes
Next Steps
Once you receive an HCC diagnosis, you are encouraged to find a doctor or cancer center with extensive experience treating it. The team approach is important because you typically have two conditions to manage: HCC and underlying liver disease. Experts on your team will accurately diagnose and stage the cancer, plan effective treatment, address the underlying condition and coordinate supportive care to help manage side effects. If you do not have access to an expert, seek a second opinion or ask your doctor to connect you with an expert for a consultation.
Another component of an HCC diagnosis is something you, your loved ones and caregivers may encounter known as disease stigma. It often accompanies HCC diagnoses because of the associated underlying conditions of the disease that may be related to lifestyle choices. It can make you feel embarrassed or ashamed, causing you to withdraw from friends, family and even medical appointments.
Most cancer centers and hospitals employ supportive care specialists who can address disease stigma along with other emotional, practical and spiritual aspects of your diagnosis. Advocacy and support groups can offer additional resources and can connect you with other people who are facing HCC. No one should have feelings of guilt about cancer, regardless of lifestyle choices.


