Advanced Breast Cancer
Overview & Staging
Your world changes when you hear you have advanced breast cancer. Whether your cancer was diagnosed as metastatic or it has recurred or progressed from an early stage, give yourself time to absorb the news — then look for ways to empower yourself. It may help to know you are not alone. The advanced breast cancer community is a close-knit, knowledgeable group of survivors, health care professionals and advocates who are ready and willing to guide and support you.
WHERE DO YOU BEGIN?
To feel more in charge of your situation, it may help to identify the parts of your life you can control. Use these suggestions to get started.
1. Find a doctor/treatment center with expertise in treating your type or subtype of breast cancer.
2. Seek a second opinion. Different doctors may have different recommendations based on their experience.
3. Learn as much as you can about your diagnosis.
4. Surround yourself with support. Draw on the people in your life who support you, then connect with other survivors in online and in-person support groups.
5. Get to know your case manager or social worker.
Understanding an Advanced Breast Cancer Diagnosis
Advanced breast cancer is a diagnosis that applies to locally advanced and metastatic disease. Locally advanced describes breast cancer that has progressed but not yet spread outside the breast or beyond local lymph nodes. This is typically Stage III and is treated with curative intent. Metastatic breast cancer describes malignant (cancerous) cells that began in breast tissue that have broken away and traveled through the bloodstream or lymph vessels to one or more distant sites in the body. When that occurs, cancer is staged as or upgraded to Stage IV.
After the lymph nodes, the most common sites of metastasis for breast cancer are the bones, lungs, brain and liver. No matter where it spreads, it is still considered breast cancer and will be treated as such.
Also referred to as metastatic breast cancer or Stage IV disease, advanced breast cancer may be detected upon diagnosis (that is referred to as de novo). It may also be found in a follow-up exam after treatment for early-stage breast cancer or because of new symptoms.
Because a cure for metastatic breast cancer is not available at this time, your treatment goal is to slow the cancer’s growth or stop its progression for as long as possible while managing side effects. Keep in mind that not all advanced breast cancers are the same. Multiple subtypes of breast cancer have been identified, and researchers continue to find differences in the ways these breast cancers grow and respond to treatment. These advances are enabling many people with advanced breast cancer to manage their disease and live happy, full lives.
Following are some types of breast cancer that have the potential for metastasizing:
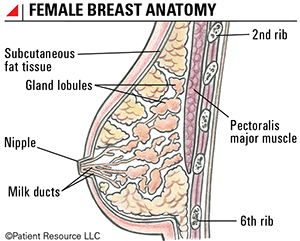
- Invasive ductal carcinoma, the most common, starts in the lining of the milk ducts in the breast when abnormal cells grow out of control, forming a mass that spreads from the ducts to normal breast tissue.
- Invasive lobular carcinoma, the second most common, starts in the lobules (glands that make milk) and spreads to surrounding normal tissue.
- Inflammatory breast cancer (IBC) is a rare, very aggressive form that grows rapidly and is automatically classified as Stage III or Stage IV, depending on whether it has spread. IBC tends to spread quickly, making it challenging to treat. Most cases are invasive ductal carcinomas in which cancer cells block the lymph vessels, causing the lymph fluid to build up. This results in breast tenderness, swelling, redness and pain. Breast skin can thicken and appear pitted like an orange peel.
Staging and Classification
The tumor, node and metastasis (TNM) system developed by the American Joint Committee on Cancer (AJCC) is used to stage and classify breast cancer (see Tables 1 and 2). The system includes the tumor (T) size, cancer cells found in nearby lymph nodes (N) and cancer that has metastasized (M), or spread, to other parts of the body, such as the bones, brain, liver or lungs.
Genomic testing is ordered to look for biomarkers — specific genes or proteins in or on cancer cells. The biomarker expression is critical in determining the type and subtype of the cancer as well as defining treatment.
The most common biomarkers in breast cancer are the hormone receptors estrogen ( ER ) and progesterone ( PR ), as well as receptors for human epidermal growth factor receptor-2 (HER2). Each can be positive ( ER +, PR + and HER2 +) or negative ( ER -, PR - and HER2 -) and in various combinations.
Patients with advanced breast cancer generally need a biopsy of the metastatic site(s) to confirm the diagnosis as breast cancer and not a second cancer, and to assess biomarkers on tissue samples of areas where the breast cancer has spread.
Your doctor may order multi-gene panels on the primary tumor to help understand how the cancer may behave and help determine which therapies may be most effective in slowing the cancer’s growth or stopping progression.
Once all these factors, including the results of a biopsy, imaging scans and genomic testing, are taken into consideration and after the breast cancer is classified, it is staged.
If You Learn Your Breast Cancer is Hereditary...
…informing your family is critical. People who have inherited abnormalities in some breast cancer-related genes have an increased likelihood of developing breast cancer and/or ovarian cancer.
The BReast CAncer 1 ( BRCA1 ) and BReast CAncer 2 ( BRCA2 ) genes are the most common hereditary susceptibility genes, and your doctor may test for others. Newly-diagnosed breast cancer patients found to have a BRCA mutation face an increased risk of another new breast cancer.
Having an inherited mutation means the risk of developing cancer is increased. There are ways to lower the risk, such as preventive surgery, medication or lifestyle changes. Frequent screenings will most likely result in early detection.
Risk factors that suggest a person carries the BRCA mutation include a family history of any cancer or multiple cancers, especially rare cancers, ovarian and male breast cancers, cancer at an early age, triple-negative ( ER -, PR -, HER2 -) breast cancer (TNBC), certain ancestry (such as Ashkenazi Jewish heritage), and a personal history of TNBC.
Table 1. AJCC TNM System for Classifying Breast Cancer
| Category | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
| T0 | No evidence of primary tumor. |
| Tis (DCIS) | Ductal carcinoma in situ. |
| Tis (Paget) | Paget disease of the nipple NOT associated with invasive carcinoma and/or carcinoma in situ (DCIS) in the underlying breast parenchyma (tissue). |
| T1 | Tumor ≤ (not more than) 20 mm in greatest dimension. |
| T1mi | Tumor ≤ (not more than) 1 mm in greatest dimension. |
| T1a | Tumor > (more than) 1 mm but ≤ (not more than) 5 mm in greatest dimension. |
| T1b | Tumor > (more than) 5 mm but ≤ (not more than) 10 mm in greatest dimension. |
| T1c | Tumor > (more than) 10 mm but ≤ (not more than) 20 mm in greatest dimension. |
| T2 | Tumor > (more than) 20 mm but ≤ (not more than) 50 mm in greatest dimension. |
| T3 | Tumor > (more than) 50 mm in greatest dimension. |
| T4 | Tumor of any size with direct extension to the chest wall and/or to the skin (ulceration or macroscopic nodules). |
| T4a | Extension to the chest wall. |
| T4b | Ulceration and/or ipsilateral (on the same side) macroscopic satellite nodules and/or edema (including peau d’orange) of the skin that does not meet the criteria for inflammatory carcinoma. |
| T4c | Both T4a and T4b are present. |
| T4d | Inflammatory carcinoma. |
| Node (N) | |
| pNX | Regional lymph nodes cannot be assessed. |
| pN0 | No regional lymph node metastasis identified or ITCs (isolated tumor cells) only. |
| pN0(i+) | ITCs (isolated tumor cells) only (malignant cell clusters no larger than 0.2 mm) in regional lymph node(s). |
| pN0(mol+) | Positive molecular findings by reverse transcriptase polymerase chain reaction (RT-PCR); no ITCs (isolated tumor cells) detected. |
| pN1 | Micrometastases; or metastases in 1-3 axillary (armpit) lymph nodes; and/or clinically negative internal mammary nodes with micrometastases or macrometastases by sentinel lymph node biopsy. |
| pN1mi | Micrometastases (approximately 200 cells, larger than 0.2 mm, but none larger than 2.0 mm). |
| pN1a | Metastases in 1-3 axillary (armpit) lymph nodes, at least one metastasis larger than 2.0 mm. |
| pN1b | Metastases in ipsilateral (on the same side) internal mammary sentinel nodes, excluding ITCs (isolated tumor cells). |
| pN1c | pN1a and pN1b combined. |
| pN2 | Metastases in 4-9 axillary (armpit) lymph nodes; or positive ipsilateral (on the same side) internal mammary lymph nodes by imaging in the absence of axillary lymph node metastases. |
| pN2a | Metastases in 4-9 axillary (armpit) lymph nodes (at least one tumor deposit larger than 2.0 mm). |
| pN2b | Metastases in clinically detected internal mammary lymph nodes with or without microscopic confirmation; with pathologically negative axillary (armpit) nodes. |
| pN3 |
Metastases in 10 or more axillary (armpit) lymph nodes;
or in infraclavicular (below the clavicle) (Level III axillary) lymph nodes; or positive ipsilateral (on the same side) internal mammary lymph nodes by imaging in the presence of one or more positive Level I, II axillary lymph nodes; or in more than three axillary lymph nodes and micrometastases or macrometastases by sentinel lymph node biopsy in clinically negative ipsilateral internal mammary lymph nodes; or in ipsilateral supraclavicular (above the clavicle) lymph nodes. |
| pN3a |
Metastases in 10 or more axillary (armpit) lymph nodes (at least one tumor deposit larger than 2.0 mm);
or metastases to the infraclavicular (below the clavicle) (Level III axillary) lymph nodes. |
| pN3b | pN1a or pN2a in the presence of cN2b (positive internal mammary nodes by imaging);
or pN2a in the presence of pN1b. |
| pN3c | Metastases in ipsilateral (on the same side) supraclavicular (above the clavicle) lymph nodes. |
| Note: (sn) and (f) suffixes should be added to the N category to denote confirmation of metastasis by sentinel node biopsy or FNA/core needle biopsy respectively, with NO further resection of nodes. | |
| Metastasis (M) | |
| M0 | No clinical or radiographic evidence of distant metastases. |
| cM0(i+) | No clinical or radiographic evidence of distant metastases in the presence of tumor cells or deposits no larger than 0.2 mm detected microscopically or by molecular techniques in circulating blood, bone marrow, or other nonregional nodal tissue in a patient without symptoms or signs of metastases. |
| cM1 | Distant metastases detected by clinical and radiographic means. |
| pM1 | Any histologically proven metastases in distant organs; or if in non-regional nodes, metastases greater than 0.2 mm. |
Table 2. Stages of Advanced Breast Cancer
| Classification | Definition |
| IIIA |
T0-T3, N2, M0
T3, N1, M0 |
| IIIB | T4, N0-N2, M0 |
| IIIC | Any T, N3, M0 |
| IV | Any T, Any N, M1 |
Advanced Breast Cancer Staging Illustrations