Cancer Immunotherapy
Melanoma
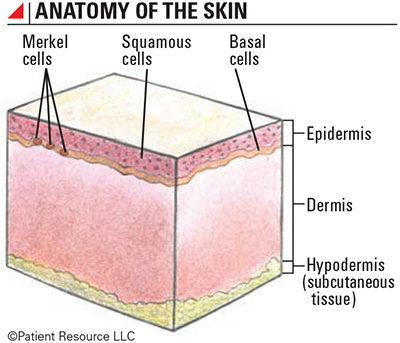
Some of the first types of immunotherapy approved by the Food and Drug Administration (FDA) for treating cancer were for melanoma. These approvals offered hope and durable responses to many who had Stage III and IV diagnoses, which had a poor prognosis, were difficult to treat and often spread quickly. Since then, the FDA has approved more immunotherapy drugs for both melanoma and other skin cancers, including cutaneous squamous cell and Merkel cell skin cancers. These drugs are considered breakthrough therapies that are offering a new way of treating these types of cancer.
Today, many immunotherapy options are available for people with melanoma. These include cytokines, immune checkpoint inhibitors and oncolytic virus therapy, which all work on different aspects of the immune system.
You may be a candidate for immunotherapy if you meet certain criteria. If you have a pre-existing autoimmune disorder, be sure to discuss it with your doctor. But immunotherapy is not effective for every person, even if it is approved for that person’s cancer type. Scientists are studying patient responses to immunotherapy to find out why. Researchers are also investigating other methods for using the immune system to fight cancer to improve the effectiveness of this treatment.
Understanding the Variety of Immunotherapy Options Available
Using immunotherapy to treat melanoma is a significant leap forward. The introduction of this new class of drugs has changed how doctors treat these cancers, and it has improved the prognosis for many people with Stage III or IV disease. Some of the very first types of immunotherapy approved were for melanoma, and it remains a cancer that generally responds well to this treatment.
Research has discovered multiple ways to harness the potential of the body’s own immune system and enable it to recognize and eliminate cancer cells. Today, several types of immunotherapy are approved to treat melanoma and other skin cancers, and all are a result of the research done in clinical trials.
Once considered a last resort for metastatic cancers, immunotherapy is often being used as a first-line therapy or second-line therapy. First-line therapy, also known as induction therapy, primary therapy and primary treatment, is the first treatment given and is usually part of the standard of care. Second-line therapy is treatment given after the primary treatment (first-line therapy) doesn’t work or stops working. Some may be used as systemic or local treatments. Systemic treatments travel throughout your body, and local treatments are injected into a lesion or applied topically to the skin.
For early stage melanoma, treatment usually involves surgery only. For more advanced stages, additional treatment options may be necessary to prevent recurrence or to treat a metastasis. Immunotherapy strategies may be given after surgery (adjuvant treatment) with the goal of reducing the risk of disease recurrence. In more advanced cases or when the cancer is unresectable (unable to be removed with surgery), immunotherapy may be used as the first-line therapy. It may also be used in combination with other treatments such as chemotherapy, targeted therapy and radiation therapy.
Research in clinical trials is ongoing to determine if immunotherapy drugs approved for Stage III and IV cancers can be used in earlier stages and to discover new types of effective immunotherapy.
The following types of immunotherapy are approved to treat melanoma.
Cytokines
Cytokine immunotherapy aids in immune cell communication and plays a big role in the full activation of an immune response. This approach works by introducing large amounts of laboratory-made cytokines to the immune system to promote specific immune responses as a systemic therapy. It is also considered a non-specific immune stimulator. Three types of cytokines are used in immunotherapy.
- Interleukins help regulate the activation of certain immune cells. They are considered a first-generation immunotherapy.
- Interferons boost the ability of certain immune cells to attack cancer cells. They are also a first-generation immunotherapy and may be given as adjuvant therapy (given after primary treatment).
- Granulocyte-macrophage colony stimulating factors (GM-CSFs) stimulate the bone marrow, promoting the growth of immune and blood cells and the development of dendritic cells, which become antigen-presenting cells (cells that show the antigens to T-cells). An oncolytic virus that includes the GM-CSF cytokine to help activate a strong immune response is approved for melanoma treatment.
Immune Checkpoint Inhibitors
This type of immunotherapy was first approved in 2011 for melanoma. These drugs are given as an infusion intravenously (IV) and are systemic. Some immune checkpoint inhibitors are approved to be used alone or in combination.
To understand how immune checkpoint inhibitors work, it is helpful to know how the immune system works in general. Because one of the primary functions of the immune system is to determine which cells or substances are self (normal) or non-self (foreign), the immune system contains cells, called B-cells and T-cells, which can recognize the foreign cells. These cells are part of the white blood cells that fight infections and eliminate cancer cells in the body. To prevent attack on normal cells, the immune system has a complex process that regulates the activity of B-cells and T-cells. The immune cells are rapidly activated to clear an infection or kill a cancer cell. However, to prevent an attack on normal cells, the immune system must slow down. It does this through the use of checkpoints.
Checkpoints keep the immune system “in check” by turning off immune cells or killing the immune cells. This may be normal after an infection has been cleared, but, in cancer, this may occur prematurely, allowing the cancer to continue to grow. In addition to checkpoints found on immune cells, other cells called regulatory T-cells may also turn down activated immune cells. When the correct checkpoint proteins and cell receptors connect, a series of signals is sent to the immune system to slow down once an immune response is finished. So far, three checkpoint receptors that slow down the immune system have been identified for their roles in cancer treatment.
- CTLA-4 (cytotoxic T-lymphocyte-associated protein 4) is a receptor that binds with certain molecules to tell the immune system to slow down.
- PD-1 (programmed cell death protein 1) is a receptor involved with telling T-cells to die and reducing the death of regulatory T-cells (suppressor T-cells). Both of these effects slow down an immune response. PD-1 can tell the immune system to slow down only if it connects with PD-L1.
- PD-L1 (programmed death-ligand 1) is a protein that, when combined with PD-1, sends a signal to reduce the production of T-cells and enable more T-cells to die.
When PD-1 (the receptor) and PD-L1 (the protein) combine, the reaction signals it’s time to slow down. CTLA-4, however, can connect with more than one protein, which is a more complex reaction than with PD-1 and PD-L1. When CTLA-4 combines with any of the various proteins, it also tells the immune system to slow down.
Checkpoint inhibiting drugs prevent connections between checkpoints. This prevents the immune response from slowing down, which allows the immune cells to continue fighting the cancer. When an immune checkpoint inhibitor is given, the immune system can better recognize cancer cells as foreign cells.
The following immune checkpoint inhibitors are currently approved as cancer treatments.
- Anti-CTLA-4 antibodies allow T-cells to continue fighting cancer cells instead of shutting down.
- Anti-PD-1 drugs allow for the continued or increased production of T-cells and enable them to continue fighting cancer.
- Anti-PD-L1 molecules prevents the destruction of T cells allow the T-cells to recognize tumor cells as the enemy and then attack them.
The approved immune checkpoint inhibitors are monoclonal antibodies (mAbs). Antibodies (a type of protein) are the body’s way of tagging a specific antigen (foreign substance). They bind to the antigen, which allows the rest of the immune system to recognize the antigen as foreign and target it for destruction.
Laboratory-made antibodies that are designed to target specific tumor targets, such as antigens or other proteins found on the cancer cell, can work in different ways, including flagging targeted cancer cells for destruction, blocking growth signals and receptors, and delivering other therapeutic agents directly to targeted cancer cells. They can also be created to carry cancer drugs, radiation particles or laboratory-made cytokines (proteins that enable immune cells to send messages to each other) directly to cancer cells. Combining mAbs with radiation particles, a treatment known as radioimmunotherapy, allows for radiation to be delivered in lower doses over a longer period of time. This direct form of radiation delivery typically damages only the targeted cells.
Oncolytic virus immunotherapy
An oncolytic virus immunotherapy uses viruses that directly infect tumor cells to cause an immune response. It is typically given as a local treatment directly to the cancer. One oncolytic virus uses a weakened version of the herpes simplex virus. It has been changed from the original and contains the GM-CSF cytokine. The virus targets specific cancer cells, infects them and duplicates itself continuously within the cell until it ruptures. This rupture kills the cell and releases the GM-CSF cytokine produced by the virus to promote an overall immune boost. This process increases the chance that the attack can also begin killing cancer cells that have not been infected with the virus. Other viruses are being evaluated as potential cancer treatments.
Vaccinations
Two types of vaccines are used against cancer: preventive vaccines and treatment vaccines. A treatment vaccine that is injected into the body to create an immune response is currently being tested in patients with melanoma.
Identifying Biomarkers to Detect Response to Immunotherapy
Now that research has shown that most cancer is caused by genetic changes in DNA, detecting these changes at the microscopic level with biomarkers is becoming an increasingly valuable part of diagnosing and treating melanomas. As a result, the use of biomarkers is expanding rapidly. Biomarkers are substances, such as genes, proteins or molecules, produced by cancer cells or other cells in the body. Biomarkers are also called tumor markers, molecular markers, biological markers or serum markers. Other biomarkers may be cells, especially immune cells. There is evidence that certain T-cells, for example, when found at higher numbers in melanoma tumors are associated with better prognosis and responses to immunotherapy.
Biomarkers may be prognostic, predictive or diagnostic. A prognostic biomarker provides information about a person’s overall cancer outcome, regardless of therapy, while a predictive biomarker gives information about the effect of a specific treatment approach. Diagnostic biomarkers help determine the type of tumor.
The following biomarkers are currently being used by some doctors to make immunotherapy treatment decisions for melanoma.
- Lactate dehydrogenase (LDH) is the only accepted serum biomarker for melanoma, and it is tested to determine if a person has an elevated risk for metastasis. A decrease in LDH has been associated with response to immunotherapy. It is a prognostic biomarker that may be elevated if the cancer has progressed. It is released when melanoma cells are damaged or die.
- PD-L1 expression may be tested to determine if the tumor cells or immune cells in the tumor’s microenvironment contain a higher level, which may mean that a patient could be a good candidate for immune checkpoint inhibitors. However, testing this biomarker alone is not sufficient to determine a therapeutic response to immunotherapy in patients with melanoma.
- Tumor mutational burden (TMB) is an assessment of the number of genetic mutations in a tumor. It can help doctors determine if a patient will respond to immunotherapy. It is believed that the higher the TMB level is, the more likely the patient will respond to immunotherapy.
- Tumor-infiltrating T-cells (TILs) are determined on biopsy and melanomas with higher numbers of TILs and those with TILs inside the tumor have been shown to have a better prognosis and may respond better to immunotherapy. Some treatments result in higher TILs and may be a biomarker for response with these therapies.
Doctors are also genetically testing melanoma tumors to identify subtypes and certain genetic mutations and to determine if any may predict if a person will respond to immunotherapy. This information aids your doctor in making treatment decisions. Some of the genetic factors that may be used more in the future to determine how a person will respond to treatment include BRAF (pronounced BEE-raff), NRAS (pronounced EN-rass) and NF1 mutations. Targeted therapies have been developed to treat BRAF mutations, specifically BRAF V600, and more are expected in the future.
Not all patients who receive immunotherapy respond, and research is ongoing to find out why. Scientists are looking for more biomarkers that may indicate whether a patient is a good candidate for immunotherapy. Biomarkers are expected to be considered more commonly in the future so that immunotherapy is not given to someone who may not respond to it.