Cancer Immunotherapy
Prostate Cancer
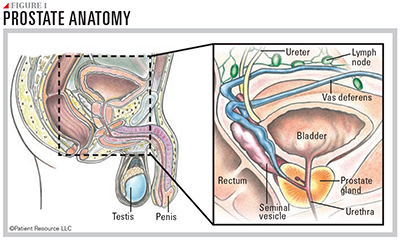
The prostate gland, which is found only in men, develops before birth and grows rapidly during puberty. In young men, it is generally the size of a walnut and continues to grow with age, as long as male hormones are present in the body.
The prostate is located below the bladder, in front of the rectum and behind the penis (see Figure 1). It surrounds the urethra (the tube that carries urine and semen out of the body through the penis), and its primary function is to produce seminal fluid, which adds liquid to semen as well as nourishes and protects sperm cells.
What is Prostate Cancer?
Prostate cancer occurs when normal cells within the prostate gland mutate and grow out of control, usually forming a tumor of abnormal cells. Most prostate cancers grow slowly and stay in the prostate. Many of these cancers can be watched carefully (active surveillance) or effectively removed or destroyed with treatment. However, some prostate cancers are aggressive. Malignant (cancerous) tumors can spread to other body parts if they are not found and treated early enough. When cancer spreads, it is likely to travel to nearby lymph nodes and then to bones and other organs. Prostate cancer that spreads is referred to as advanced prostate cancer.
Nearly all prostate cancers are adenocarcinomas, which develop in the gland cells in the prostate. A very small percentage of prostate cancers are sarcomas, small cell carcinomas, transitional cell carcinomas or neuroendocrine tumors.
More than 90 percent of prostate cancers are detected while still confined to the prostate and nearby organs, primarily due to the prostate-specific antigen (PSA) test. Early diagnosis is generally made using transrectal ultrasound (TRUS) guided biopsy.
The incidence of prostate cancer increases with age more quickly than any other cancer. It’s more common in African-American men and Caribbean men of African descent. Other factors that raise the risk of developing prostate cancer include a family history of the disease and possessing certain inherited gene mutations.
Immunotherapy for Prostate Cancer
Immunotherapy uses the body’s own immune system to recognize and attack cancer cells that have been hiding and targets them for destruction. This approach is quite different from that of other types of cancer treatments. Currently, one type of immunotherapy is approved to treat advanced prostate cancer, and it comes in the form of a vaccine.
Vaccine
Two types of vaccines are used against cancer: preventive vaccines and therapeutic (or treatment) vaccines. Preventive vaccines are given before a person develops cancer with the goal of stopping it from forming. Treatment vaccines may be given to treat existing cancers. Anti-cancer vaccines are created from either viruses or tumor cells that have been changed in a laboratory. Their goal is to direct immune cells to the cancer cells. Some of these vaccines are custom-made for the patient’s specific tumor type while others are “off-the-shelf” vaccines that contain one to more than 100 antigens that are common to the patient’s type of cancer. The first FDA-approved immunotherapy for prostate cancer is an antigen-presenting cell-based treatment vaccine specifically for metastatic castration-resistant (hormone refractory) prostate cancer.
immune cells are
extracted from
the body.

a lab, where they are
modified to recognize and
destroy cancer cells.
is created just for you.

and the modified cells
activate other immune cells
so they can recognize and
destroy the cancer cells.
You may be a candidate for this treatment if you are on hormone therapy and have a rising PSA level, if your cancer has spread from the prostate to other places in your body, and if you are not taking narcotics for cancer-related pain.
This vaccine is unique in that it is personalized for each patient. As a result, getting it involves more than simply getting an injection at the doctor’s office. It is a multi-step process that requires a commitment from the patient, especially in terms of timing. If you are considering this option to treat your advanced prostate cancer, it’s helpful to be aware of what to expect.
Treatment begins with the collection of your blood cells in a process known as leukapheresis. Your blood is passed through a machine that collects some of your immune (white blood) cells, while the rest of the blood (platelets and red blood cells) is returned to your body. This is an outpatient procedure that typically takes about three to four hours.
The blood that was collected is sent to a special facility where the white blood cells are modified to be able to recognize and destroy prostate cancer cells. A dose of the vaccine is then created especially for you.
Three or four days later, you are given the dose of the vaccine by infusion (an intravenous fluid). This is generally given on an outpatient basis in your doctor’s office or treatment center and will likely take a little more than an hour.
This entire process is repeated two more times, approximately one to two weeks apart. You will have a total of six appointments — three cell collections and three infusions. The full treatment generally takes about a month.
Once these modified white blood cells are injected back into your body, they activate cancer-killing T-cells that travel through the bloodstream looking for cancer cells to destroy. A distinct characteristic of immunotherapy is its potential to remain effective long after treatment ends, a feature called “memory.” This means the immune system can continue to seek out and attack cancer cells until they are eliminated. When your immune system encounters a virus, such as chicken pox, it automatically remembers if it is exposed to it again and offers you immunity, meaning you usually don’t get another case of chicken pox. With immunotherapy, your immune system may be able to recognize a specific type of cancer cell easier, which can lead to long-term, cancer-free remission of that type and increased overall survival. This is the same characteristic that allows a traditional vaccine, such as the tetanus vaccine, to remain effective for many years.
It is crucial to stay on schedule with the cell collection and infusion appointments. The doses are made for you only, and they have an expiration date. If you miss an appointment and don’t receive the dose when you are supposed to, you must have your cells collected again so another dose can be made especially for you. Because a missed appointment will delay treatment, you are encouraged to be diligent about keeping your appointments. Consider asking a loved one or caregiver to help you remember, or explore the many online schedules and calendar apps that are available. Many have reminder features that are very helpful.
If you need additional treatment after receiving this vaccine, other options, such as chemotherapy, hormone therapy and radiotherapy, may be available to you. More immunotherapy agents, including other types of vaccines, are currently being studied in clinical trials. For more about clinical trials, click here.
Common Side Effects
One of the potential benefits of immunotherapy is that it tends to affect only cancer cells. Other forms of treatment are more likely to affect healthy cells in addition to cancer cells. For example, surgery, chemotherapy, androgen deprivation therapy and radiation therapy kill rapidly multiplying cells, which include cancer cells as well as healthy cells that also multiply quickly, such as blood cells and cells in the gastrointestinal tract. The accompanying destruction of healthy cells and tissues contributes to common side effects, such as fatigue, nausea and vomiting, hair loss and low blood counts. Immunotherapy is different because it primarily targets cancer cells. Although there may be fewer side effects from immunotherapy than with other cancer treatments, it is realistic to expect that you will experience some.
Since these drugs work by stimulating the immune system, it’s important to pay attention to every side effect you experience. Your doctor will monitor you closely for complications during treatment, and your medical team will rely on you to communicate your side effects frequently because they may develop rapidly and may range from mild to life-threatening. Seek treatment immediately, regardless of time of day, for symptoms including high fever, inflammation, swelling, severe abdominal pain or shortness of breath.
Ask your doctor which side effects to expect with vaccine therapy and when they may happen. Some may occur right away, while others may not show up for months or years after treatment. Once you know what to watch for, ask your doctor about the best ways to prevent or treat them if they occur. When in doubt about any side effects, contact your doctor.